What happened to our health?
About the curve that stopped rising and why innovation will fix American healthcare
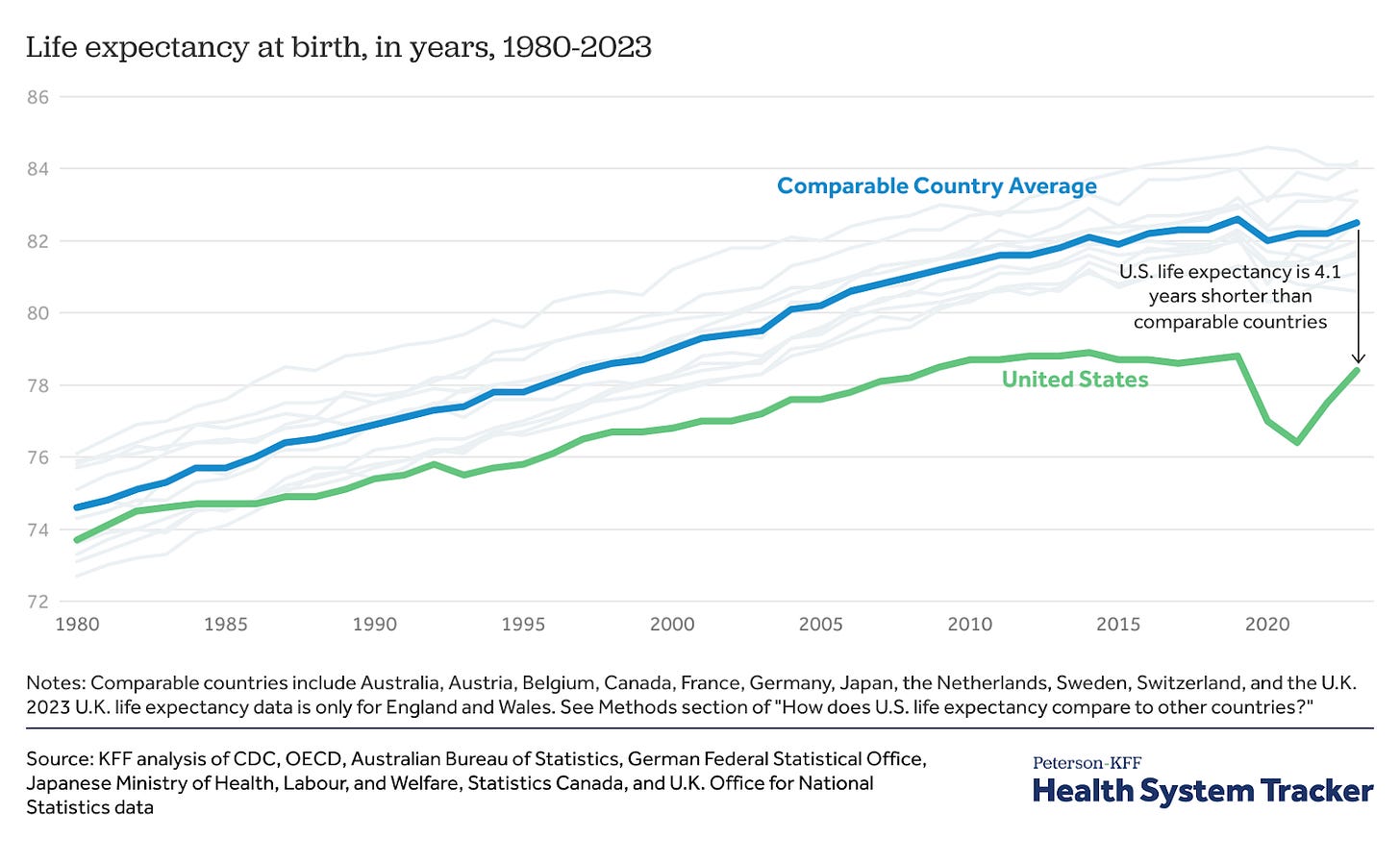
For most of the last century, America kept getting healthier. Every decade America lived longer, felt stronger, and believed the next generation would do even better. But somewhere around the turn of the millennium, that curve flattened. The question is why? Why did progress stop?
A Century of Ascent
In 1900, the average American lived just 47 years. By 1950, it was 68. By 2000, nearly 78. (CDC)
That’s a 30-year leap in a single century. One of the greatest health transformations in human history. Vaccines and antibiotics wiped out infectious disease. Clean water and sanitation became universal. America learned how to deliver babies safely, manage chronic conditions, and nourish entire populations.
For a hundred years, the health graph of America pointed relentlessly upward. Then, around 2000, it didn’t.
The Plateau
From 2000 to now, U.S. life expectancy grew only by a year, from 78 to 79. It dipped during COVID and still haven’t recovered. (CDC). For example, Between 2010 and 2019, the U.S. gained just 0.1 years of life expectancy, while peer nations gained more than a full year. (Health System Tracker)
It’s not because America stopped caring. America spends more on healthcare than any country in the world. Yet the return on that investment, such as longer, healthier lives, has stagnated. The curve that defined a century of progress has gone flat.
Two Americas
Of course, life expectancy isn’t everything. It tells us how long we live, not how well. Living to 85 but spending 20 of those years fighting chronic disease isn’t success. Quality of life matters.
And the averages hide another harsh truth. In some U.S. counties, life expectancy still reaches the 80s, while in others it’s closer to 60. (CBS News) The gap between zip codes can mean 10 to 20 years of life. (Hamilton Project)
That’s not just a plateau, but a divergence; two health trajectories inside one country.
The Innovation Slowdown
If the 20th century was about conquering infection, the 21st was supposed to be about conquering everything else that is non-infectious: cancer, Alzheimer’s, autoimmune disease. But the rate of new medical breakthroughs has slowed. Clinical trials are more expensive, slower, and riskier than ever. The industry has grown cautious, often chasing incremental gains instead of transformative cures.
Big bets are made on AI to reinvent drug discovery, which is promising. Yet discovery is only half the equation. The other half is getting those discoveries through clinical trials and into patients’ hands.
Right now, that system is broken. Trials fail too often, take too long, and cost too much. Not always because the science is weak, but rather because the data is. We need a new layer of intelligence for clinical trials. A way to make clinical trials learn faster from themselves. That’s how medicine will start compounding again.
The Real Health Equation
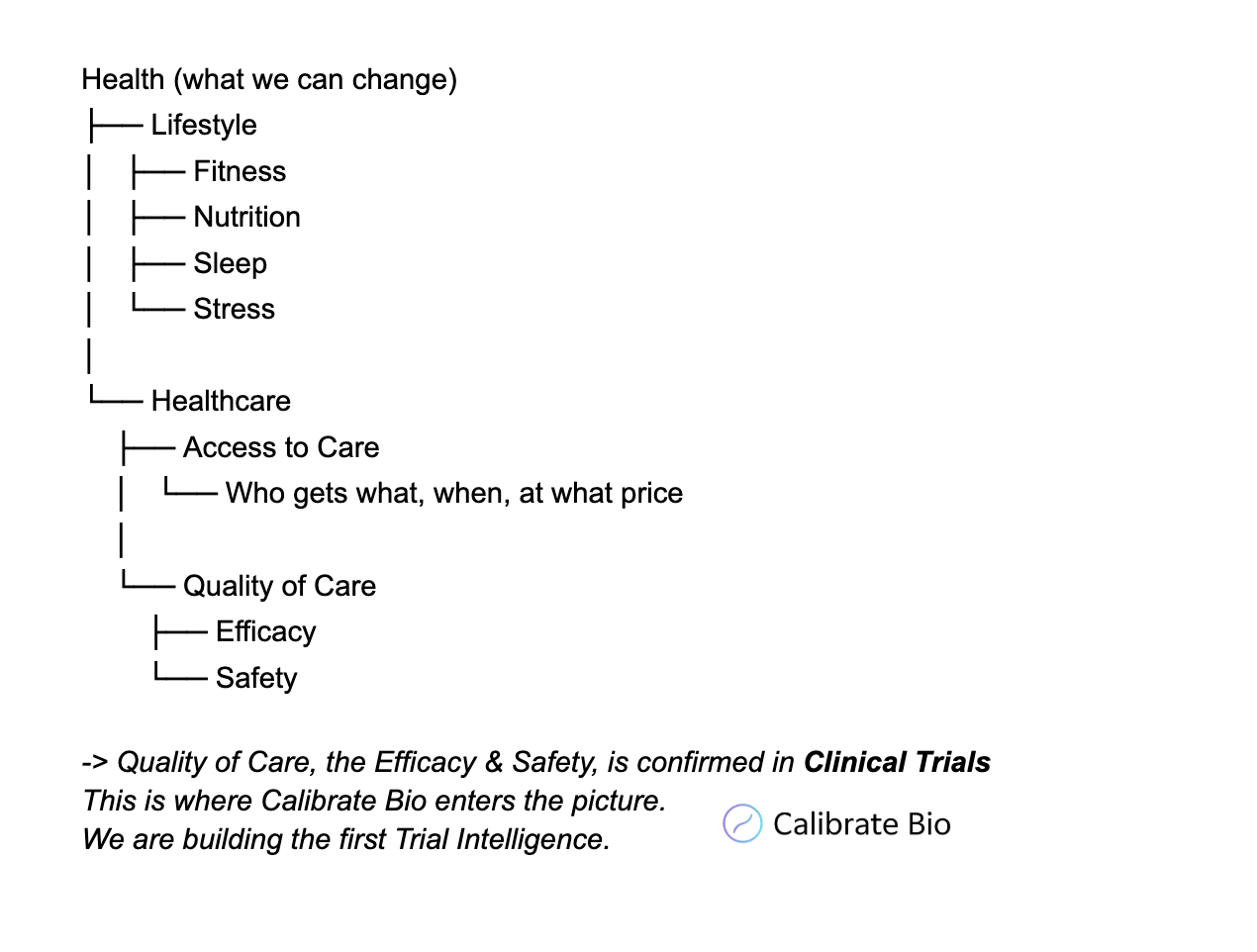
Health has many dimensions. Some we can change. Here is an overview:
Health = Lifestyle + Healthcare
Lifestyle = Fitness + Nutrition + Sleep + Stress
Healthcare = Access * Quality
Access is about policy: who gets care, when, where, at what price, and who pays for it? It’s shaped by coverage, cost, geography, and demography. Quality, on the other hand, is about how well and how safely treatments work; whether it’s a drug, surgery, or device.
Most people believe access is the main issue in American care. A lot of hardworking young people I know focus their careers on health policy and equity. This matters, but access is ultimately a political fight and in today’s divided climate, progress is tough. Quality is where we have more room to make real change. It’s the part that drives innovation. Lately, it’s stalled. The biggest issue in healthcare right now isn’t just access alone, but quality. That is because access and quality share the same root solution: a more competitive and dynamic pharmaceutical industry. More pharma companies, more innovators, more researchers becoming founders, and more overlap between pharma, biotech, and techbio startups would mean more treatments to market, more competition, and more choices. That competition would naturally drive prices down and make care more available as we wait for laws or policies to change. It’s the market’s way of creating progress now. It gives us builders agency, now, to build better healthcare, as we wait for political changes that are far from guaranteed.
The Next Health Curve
From 1900 to 2000, America built the public health systems that lifted an entire nation. From 2000 to now, America has been coasting on their legacy.
The next leap won’t come from more hospitals or more coverage alone. It will come from making the system itself smarter. Clinical trials that learn, data that connects, therapies that reach patients more intelligently.
We don’t just need more drugs. We need a better way to prove they work. That’s how we get the curve rising again. In the next article In the next article, I’ll explore what Intelligent Pharma really means. What does the future of clinical trials look like? How will the next generation of pharma, biotech, and care systems transform the way we develop and deliver treatments? A healthy future awaits us and we have the agency to deliver it sooner rather than later.
Watch: “What Happened to Our Health”: